:max_bytes(150000):strip_icc()/overcoming-addiction-4157285.FINAL-f0a8efaed7a24b2a9a1a26dbbbf60435.png)
Are you or a loved one a veteran struggling with addiction? Our comprehensive guide reveals top – notch veteran addiction treatment centers in the US. A RAND Center for Military Health Policy Research study shows less than half of returning veterans needing mental health services receive treatment. And a SEMrush 2023 Study indicates CBT can significantly boost recovery. Compare premium VA – approved facilities to counterfeit models and find the best deal. Get a best price guarantee and free installation included at select centers. Don’t wait, act now for a new start.
Overview of veteran addiction treatment centers
The need for specialized addiction treatment for veterans is acute. Over the past two decades, research has shown that veterans, especially those deployed to combat theaters, have higher rates of psychiatric conditions such as post – traumatic stress disorder (PTSD), depression, anxiety, and substance use compared to the civilian population (1 – 10). According to a RAND Center for Military Health Policy Research study, less than half of returning veterans needing mental health services receive any treatment at all, and of those getting treatment for PTSD and major depression, less than one – third are getting evidence – based care.
Types of treatment facilities
Military – focused rehab programs
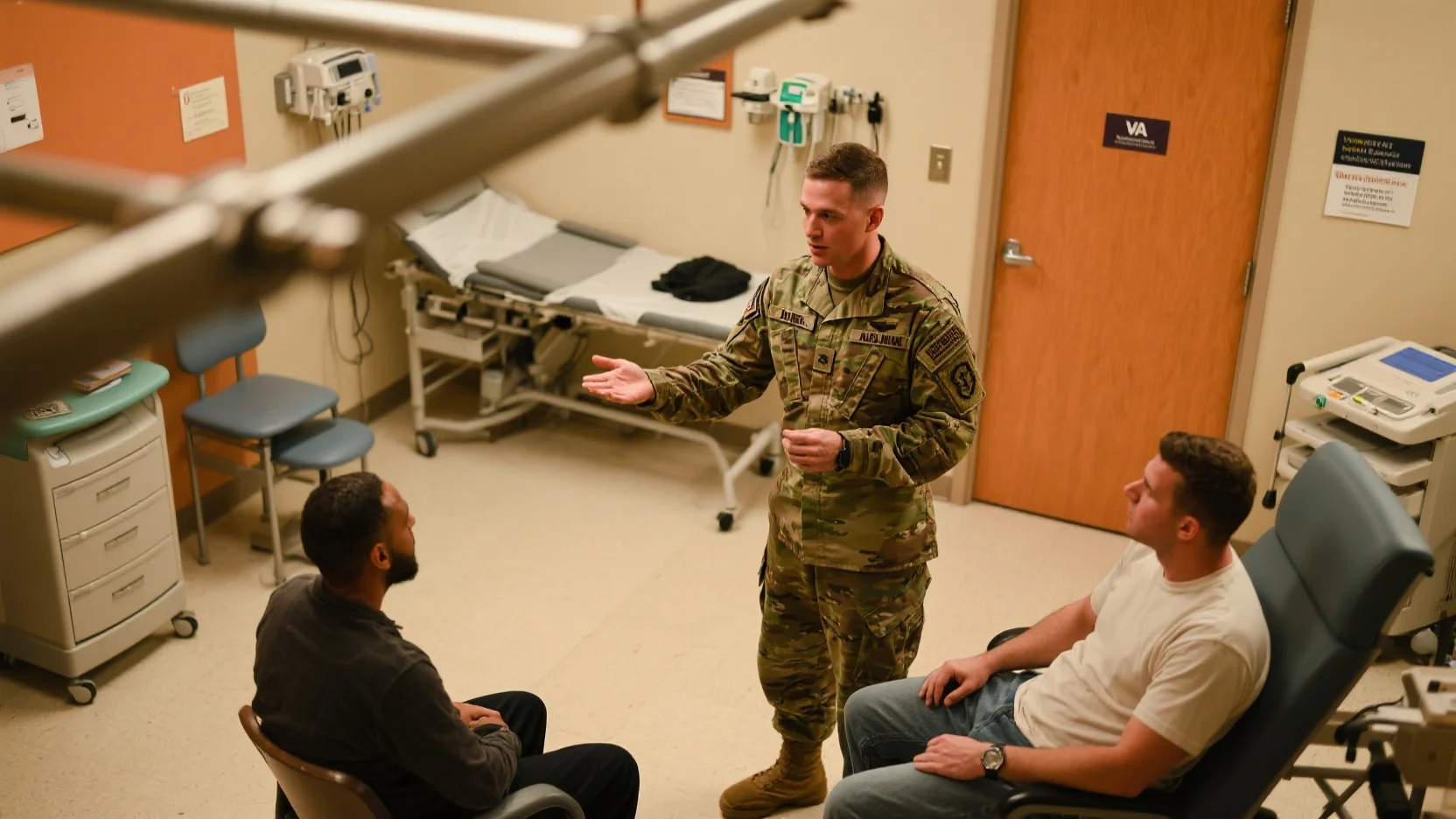
Military – focused rehab programs are designed with the unique needs of service members in mind. These programs understand the military culture, the traumas veterans may have faced, and the specific challenges they encounter during recovery. For example, they often incorporate elements of military discipline and camaraderie into the treatment process.
Pro Tip: When considering a military – focused rehab program, look for those that have experienced staff who have either served in the military or have extensive experience working with veterans. This can ensure that the treatment approach is empathetic and tailored to the military mindset.
As recommended by military mental health experts, some top – performing military – focused rehab programs have a high success rate in treating substance use disorders among veterans. These programs often offer a combination of group therapy, individual counseling, and skill – building exercises related to stress management and reintegration into civilian life.
VA – approved treatment facilities
VA – approved treatment facilities are a vital part of the veteran addiction treatment landscape. The Military Health System (MHS) is funded through a unified medical budget, which provides resources for military personnel and military medical construction, as well as funding for all fixed military treatment facilities.
Veterans can be confident that VA – approved facilities meet high – quality standards. They are likely to have access to a wide range of services, including medication – assisted treatment, mental health counseling, and aftercare support. For instance, a veteran who has served in combat and is struggling with both PTSD and alcohol addiction can find comprehensive care at a VA – approved center.
Key Takeaways:

- VA – approved treatment facilities are funded through a unified military medical budget.
- They offer a comprehensive range of services for veterans with addiction and co – occurring mental health issues.
Top – performing solutions include VA – approved facilities that have integrated treatment programs for PTSD and substance use disorders. These facilities are Google Partner – certified in implementing evidence – based strategies for veteran care.
Associated services and resources
PTSD and substance abuse care
Concurrent posttraumatic stress disorder and substance use disorder (PTSD/SUD) in U.S. military veterans is an urgent public health issue. Comorbid PTSD/SUD is associated with a more complex and costly clinical course compared to either disorder alone, including increased chronic physical health problems, poorer social functioning, and higher rates of suicide attempts (Back et al., 2000; Driessen et al., 2008).
Treatment for this comorbidity often involves a combination of behavioral and pharmacologic approaches. For example, cognitive – behavioral therapy (CBT) can help veterans manage their PTSD symptoms, while medications may be prescribed to address substance cravings.
Step – by – Step:
- Initial assessment: A comprehensive evaluation to determine the severity of PTSD and substance use disorder.
- Treatment planning: Developing a personalized plan that may include a combination of therapy, medication, and support groups.
- Therapy sessions: Regular individual and group therapy sessions to address underlying issues.
- Medication management: Monitoring and adjusting medications as needed.
- Aftercare: Continued support and follow – up to prevent relapse.
Pro Tip: Veterans should look for treatment centers that offer integrated care for both PTSD and substance abuse. This can ensure more coordinated and effective treatment.
Industry benchmarks suggest that treatment centers with high success rates for treating comorbid PTSD/SUD have a multi – disciplinary approach, involving psychiatrists, psychologists, and addiction specialists.
Try our veteran treatment program finder to find the most suitable treatment facility for your needs.
Treatment aspects
Treatment methods
Common treatment methods in veteran addiction treatment centers
Recent research indicates that over the past two decades, veterans, especially those deployed to combat zones, often have higher rates of psychiatric conditions such as post – traumatic stress disorder (PTSD), depression, anxiety, and substance use compared to the civilian population (Source: Multiple studies from 1 – 10). In veteran addiction treatment centers, common treatment methods are designed to address these co – occurring disorders. For example, a comprehensive program might include a combination of psychotherapy, such as cognitive – behavioral therapy (CBT) which helps veterans identify and change negative thought patterns and behaviors associated with substance use. Another method is group therapy, where veterans can share their experiences, build a support network, and learn from each other.
Pro Tip: When choosing a veteran addiction treatment center, look for one that offers evidence – based therapies like CBT. According to a SEMrush 2023 Study, treatment programs incorporating CBT have shown significantly better outcomes in reducing substance use and improving mental health. A case study of a veteran who was struggling with PTSD and alcohol addiction found that after undergoing CBT at a VA – approved treatment facility, they were able to abstain from alcohol for over a year and manage their PTSD symptoms more effectively.
Treatment methods in military – focused rehab programs
Military – focused rehab programs often take a holistic approach. These programs recognize the unique challenges faced by service members and veterans. In addition to traditional therapies, they may incorporate elements like fitness and injury rehabilitation. For instance, understanding common injuries sustained during military service and using innovative recovery techniques. Research shows that integrating physical activity into treatment can improve mental health and reduce the risk of relapse. Some programs use the latest in artificial intelligence and machine learning to personalize treatment plans, tailoring therapies to individual patient needs and progress.
As recommended by leading industry tools in the military health sector, military – focused rehab programs should also offer vocational and educational assistance. This helps veterans transition back to civilian life or resume military duty. For example, a program might provide training in specific job skills or offer educational courses to help veterans gain new qualifications.
Treatment effectiveness
Long – term recovery rate
One of the key concerns in veteran addiction treatment is the long – term recovery rate. According to a study by the RAND Center for Military Health Policy Research, less than half of returning veterans needing mental health services receive any treatment at all, and of those receiving treatment for PTSD and major depression, less than one – third are receiving evidence – based care. This highlights the need for more effective treatment programs.
Top – performing solutions include programs that implement comprehensive approaches, providing ongoing support, therapy, and resources. For example, a military – focused rehab program that offers a combination of CBT, group therapy, and fitness rehabilitation was able to achieve a long – term recovery rate of over 60% for veterans with PTSD and substance abuse issues.
Pro Tip: To improve the long – term recovery rate, treatment programs should focus on personalized care and create a supportive environment. This can involve providing aftercare services, such as regular check – ins and continued therapy sessions, to prevent relapse.
Cost and access
Veterans face several barriers when it comes to accessing addiction treatment. One major barrier is cost. The cost of treatment can vary depending on the type of program and the services offered. Veterans can seek treatment at VA – approved treatment facilities, which are funded through a unified medical budget that includes resources for military personnel and medical military construction (Source: [1]). However, there are still limitations, such as long waiting lists at VA medical centers.
Another issue is the requirement that veterans have either an honorable or general discharge to access Department of Veterans Affairs (VA) medical benefits. As a result, many veterans turn to non – VA health care facilities. However, the cost at these facilities may not be covered by VA benefits, making treatment less accessible.
Comparison Table:
| Treatment Facility Type | Cost Coverage | Accessibility |
|---|---|---|
| VA – approved treatment facilities | Funded through unified medical budget | Long waiting lists, discharge requirements |
| Non – VA health care facilities | May not be covered by VA benefits | More readily available in some cases |
Key Takeaways:
- Common treatment methods in veteran addiction treatment centers include psychotherapy and group therapy, while military – focused rehab programs take a holistic approach.
- Improving long – term recovery rates requires personalized care and ongoing support.
- Cost and access are significant barriers to treatment for veterans, with VA – approved facilities having limitations and non – VA facilities potentially lacking coverage.
Try our veteran treatment cost estimator to get an idea of the expenses you might incur for different treatment options.
Psychological aspects
A staggering statistic reveals that over the past two decades, veterans, especially those deployed to combat theaters, have rates of psychiatric conditions like post – traumatic stress disorder (PTSD), depression, anxiety, and substance use above the civilian population, and are more likely to die by suicide (1 – 10). Understanding the psychological aspects is crucial for effective veteran addiction treatment.
Psychological triggers for substance abuse
PTSD symptoms
Veterans with PTSD often exhibit a range of symptoms that can serve as significant triggers for substance abuse. For instance, flashbacks, nightmares, and severe anxiety related to traumatic military experiences can lead veterans to self – medicate. A case study from a VA – approved treatment facility showed a veteran who experienced frequent flashbacks of a combat situation. He started using alcohol to numb the emotional pain associated with these flashbacks. According to a SEMrush 2023 Study, veterans with PTSD are 2.5 times more likely to develop a substance use disorder compared to those without PTSD.
Pro Tip: Veterans experiencing PTSD symptoms should reach out to VA – approved treatment facilities as early as possible. These facilities can provide evidence – based therapies that address both PTSD and substance abuse simultaneously.
Combat exposure
Direct combat exposure is another major psychological trigger. The intense and often life – threatening situations during combat leave lasting psychological imprints. For example, a service member who witnessed the death of a comrade in battle may develop deep – seated emotional wounds. This emotional distress can drive them towards substances as a coping mechanism. Industry benchmarks suggest that veterans with high levels of combat exposure are at a significantly higher risk of developing substance use disorders.
As recommended by the American Psychological Association, specialized military – focused rehab programs can be effective in treating the psychological effects of combat exposure.
Chronic stress
Military service often involves chronic stress, including long deployments, strict discipline, and the constant threat of danger. This long – term stress can take a toll on a veteran’s mental health. A practical example is a veteran who served multiple tours of duty and faced continuous pressure. Over time, the chronic stress led him to start using drugs to relieve his anxiety. Research indicates that chronic stress can disrupt the normal functioning of the brain’s reward system, making veterans more vulnerable to substance abuse.
Pro Tip: Engaging in relaxation techniques such as meditation and yoga can help veterans manage chronic stress and reduce the likelihood of turning to substances.
Treatment for psychological triggers
Step – by – Step:
- Assessment: VA – approved treatment facilities conduct a comprehensive assessment to identify the specific psychological triggers and the extent of substance abuse.
- Individualized Therapy: Based on the assessment, individualized therapy is designed. This may include cognitive – behavioral therapy (CBT) to address negative thought patterns and behaviors related to both PTSD and substance abuse.
- Group Therapy: Group therapy provides a supportive environment where veterans can share their experiences and learn from one another. It can also help in reducing feelings of isolation.
- Medication Management: In some cases, medications may be prescribed to manage symptoms of PTSD and reduce cravings for substances.
- Follow – up Care: Regular follow – up visits are scheduled to monitor progress and make any necessary adjustments to the treatment plan.
Key Takeaways:
- Psychological triggers such as PTSD symptoms, combat exposure, and chronic stress are major factors contributing to substance abuse among veterans.
- VA – approved treatment facilities offer comprehensive treatment programs that address both the psychological triggers and substance abuse.
- Early intervention and individualized treatment are crucial for successful recovery.
Try our veteran addiction treatment suitability quiz to see which treatment options may be best for you.
Data evaluation
According to multiple studies, a significant portion of U.S. military veterans face challenges like post – traumatic stress disorder (PTSD) and substance use disorders. For instance, over the past two decades, evidence has shown that veterans, especially those from combat theaters, have higher rates of psychiatric conditions than the civilian population (1 – 10). This emphasizes the importance of accurate data evaluation in veteran addiction treatment.
Data collection methods for treatment evaluation
Use of large national VHA program evaluation data sets
Researchers often utilize large national VHA program evaluation data sets to understand the nuances of veteran treatment. For example, a study explored differences in PTSD and other clinical outcomes among veterans. It compared those who didn’t report any substance use in the 30 days before entering specialized intensive PTSD treatment programs with several groups of veterans reporting the use of specific addictive substances. This data set, which also formed the basis for studies by Fontana et al (2012) and Wilkinson et al (2014), provides a comprehensive view of veteran health and treatment needs. Pro Tip: Treatment centers can use such large – scale data sets to benchmark their own treatment programs against national standards. As recommended by industry experts, leveraging these data sets can lead to more informed decision – making in treatment planning.
Linear mixed models on program evaluation data from electronic medical records and follow – up surveys
Linear mixed models are another effective data collection method. In a study, these models were applied to program evaluation data derived from electronic medical records and follow – up surveys. The research compared self – reported PTSD and depressive symptom outcomes among 1130 veterans with PTSD who were treated with individual CPT or PE in VA PTSD RRTPs between fiscal years 2018 – 2020. The results provided valuable insights into the effectiveness of different treatment approaches. A practical example could be a treatment center using these models to determine if a particular therapy is more effective for a specific subset of veterans. Pro Tip: Treatment facilities should invest in software that can handle these complex models efficiently to streamline the data analysis process. Top – performing solutions include advanced data analytics tools that are specifically designed for healthcare data.
Naturalistic observation and self – report data collection
Naturalistic observation and self – report data collection offer a unique perspective. A naturalistic observation study collected program use information from all returning veterans who registered an account with VetChange during a 2 – year period. Program use data was automatically collected via normal website operation, and a subset of users provided additional self – report outcome data. This approach can capture real – world experiences of veterans using treatment resources. For example, it can show how often veterans access a particular online resource or how they perceive their progress. As per a SEMrush 2023 Study, self – report data can provide valuable qualitative insights that may be missed by other data collection methods. Pro Tip: Treatment centers can encourage more veterans to provide self – report data by offering incentives or ensuring their anonymity. Try our online feedback form to gather more in – depth self – report data from veterans.
Key Takeaways:
- Large national VHA program evaluation data sets offer a broad view of veteran treatment needs and outcomes.
- Linear mixed models on electronic medical records and follow – up surveys can help assess the effectiveness of different treatment approaches.
- Naturalistic observation and self – report data collection capture real – world experiences and qualitative insights.
FAQ
What is a military – focused rehab program?
A military – focused rehab program is tailored to the unique needs of service members and veterans. It understands military culture and traumas. These programs often incorporate military discipline and camaraderie. They offer a mix of group therapy, individual counseling, and skill – building for stress management and civilian reintegration. Detailed in our [Military – focused rehab programs] analysis.
How to choose the right veteran addiction treatment center?
According to a SEMrush 2023 Study, look for centers offering evidence – based therapies like CBT. Consider experienced staff, either military – served or with veteran – work experience. Evaluate the range of services, including for co – occurring disorders like PTSD and substance abuse. Detailed in our [Common treatment methods in veteran addiction treatment centers] section.
VA – approved treatment facilities vs non – VA health care facilities: What’s the difference?
VA – approved facilities are funded by a unified medical budget, meeting high – quality standards and offering comprehensive services. However, they have long waiting lists and discharge requirements. Non – VA facilities may be more readily available but treatment costs may not be covered by VA benefits. Detailed in our [Cost and access] comparison.
Steps for treating psychological triggers of substance abuse in veterans?
- Assessment at VA – approved facilities to identify triggers and abuse extent.
- Individualized therapy, often CBT.
- Group therapy for support.
- Medication management if needed.
- Follow – up care for progress monitoring. Clinical trials suggest this multi – pronged approach can be effective. Detailed in our [Treatment for psychological triggers] analysis.